A Northwestern research team received a $200,000 grant from the National Science Foundation (NSF) to continue developing a novel wearable device and set of algorithms specifically tailored to catch early signs and monitor progression of COVID-19.

A research team led by Northwestern Engineering bioelectronics pioneer John A. Rogers has received a $200,000 grant from the National Science Foundation (NSF) to continue developing a novel wearable device and set of algorithms specifically tailored to catch early signs and monitor progression of COVID-19.
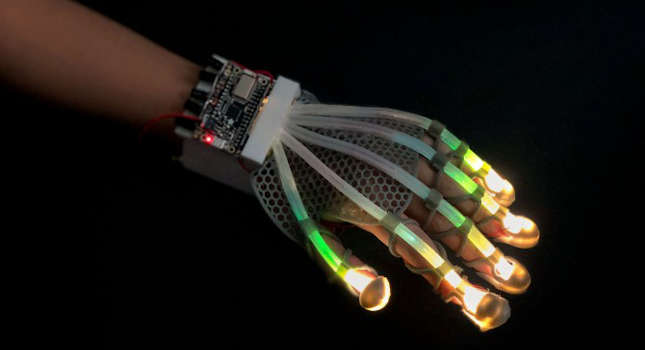
In partnership with researchers at Shirley Ryan AbilityLab, Rogers launched the device in April. The NSF funding will help Rogers and his team incorporate more advanced data analytics into the device and add a sensor to measure oxygen levels in the blood. This project is among the latest to receive a rapid response research (RAPID) grant from the NSF, which has called for immediate proposals that have potential to address the spread of COVID-19.
“Our device addresses a key issue in the COVID-19 pandemic: the limited capacity of healthcare systems,” Rogers said. “By continuously monitoring high-risk individuals, such as healthcare workers and the elderly, we can minimize the number of unnecessary hospital visits and provide an early warning to enable preventive measures.”
Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering and Biomedical Engineering in Northwestern’s McCormick School of Engineering, professor of neurological surgery in the Feinberg School of Medicine, and director of the Querrey Simpson Institute for Bioelectronics.
While low oxygen level is a key sign of COVID-19, most people don’t notice this symptom until they become very sick. This has sparked the trend of people wearing pulse oximeters at home. Whereas typical pulse oximeters clip onto a fingertip, Rogers is building this capability into his device, which sits just below the suprasternal notch on the throat. The soft, flexible, biocompatible device eliminates wires and allows continuous monitoring, even when the wearer is in the shower or exercising. Adding blood oxygen levels will help the device and its accompanying algorithms give a fuller picture of the disease’s onset, progression, and response to treatment.
To incorporate advanced data analytics into the device, Rogers is collaborating with Naresh Shanbhag, a professor of electrical and computer engineering at the University of Illinois, Urbana-Champaign. Machine-learning algorithms will help connect the device’s measurements — for cough, oxygen levels, and chest wall movements — to specific aspects of COVID-19. This will help physicians determine if a patient’s cough, for example, is caused by COVID-19 or something more benign.
Northwestern University
– Edited by Chris Vavra, associate editor, Control Engineering, CFE Media & Technology, [email protected].